Should Diaphragmatic Hernia Be Repaired If No Symptoms
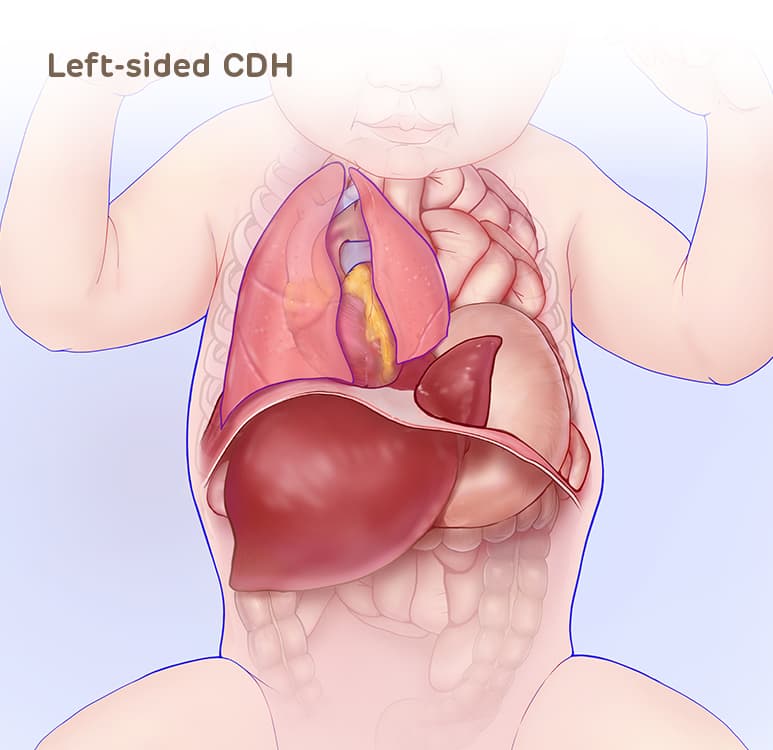
 With CDH, a hole in the diaphragm allows abdominal organs to move into the chest during fetal development. There, they can crowd the heart and lungs and keep the lungs from growing normally. © CHOP/CFDT Congenital diaphragmatic hernia (CDH) occurs when the diaphragm, the muscle that separates the chest from the abdomen, fails to close during prenatal development. This opening allows contents of the abdomen (stomach, intestines and/or liver) to migrate into the chest, impacting the growth and development of the lungs. The lungs will be smaller than expected (pulmonary hypoplasia), and will have less developed blood vessels. This causes high blood pressure in the lungs (pulmonary hypertension).
With CDH, a hole in the diaphragm allows abdominal organs to move into the chest during fetal development. There, they can crowd the heart and lungs and keep the lungs from growing normally. © CHOP/CFDT Congenital diaphragmatic hernia (CDH) occurs when the diaphragm, the muscle that separates the chest from the abdomen, fails to close during prenatal development. This opening allows contents of the abdomen (stomach, intestines and/or liver) to migrate into the chest, impacting the growth and development of the lungs. The lungs will be smaller than expected (pulmonary hypoplasia), and will have less developed blood vessels. This causes high blood pressure in the lungs (pulmonary hypertension).
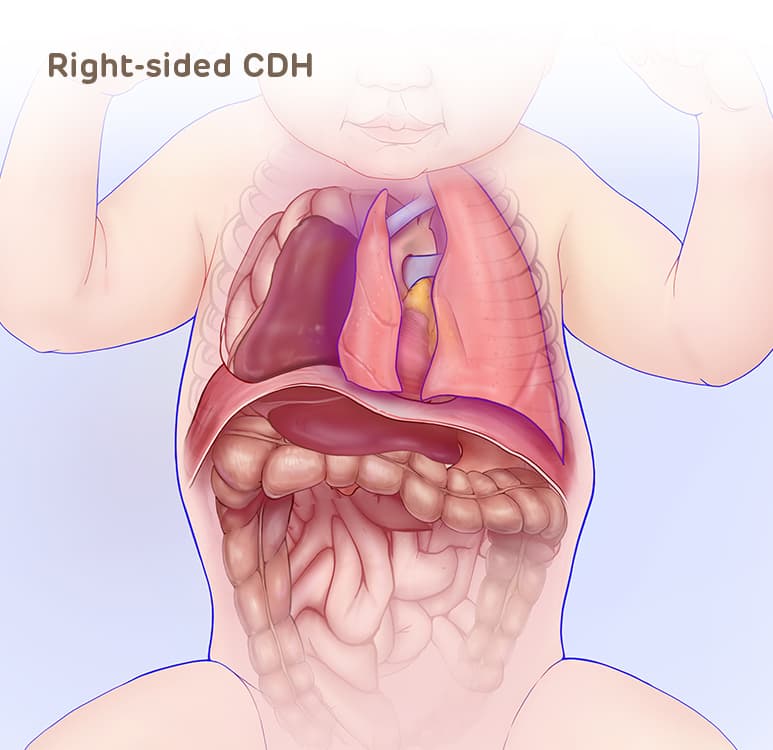
CDH is one of the most common major congenital anomalies, occurring in 1 of every 2,500 – 3,000 live births. CDH can occur on the left or right side, or rarely on both sides. Newborns affected with CDH will require immediate care at delivery, so early and accurate diagnosis is important.
View this video with a transcript
The cause of CDH is unknown. Typically CDH is an isolated finding although it can occur along with heart disease or a genetic abnormality which can lead to additional complications.
 Left-sided CDH showing the liver (highlighted) and bowel herniated into the fetal chest. © CHOP/CFDT CHOP is engaged in active research projects seeking to better understand the associations and causes of CDH. Genetic researchers are using innovative techniques to try to find the potential underlying genetic etiology of CDH. Identifying the genetic cause(s) of CDH will allow our clinicians to better manage and counsel families with an affected child.
Left-sided CDH showing the liver (highlighted) and bowel herniated into the fetal chest. © CHOP/CFDT CHOP is engaged in active research projects seeking to better understand the associations and causes of CDH. Genetic researchers are using innovative techniques to try to find the potential underlying genetic etiology of CDH. Identifying the genetic cause(s) of CDH will allow our clinicians to better manage and counsel families with an affected child.
CDH is typically discovered during a routine prenatal ultrasound. The sonographer may notice stomach, intestine, or liver in your baby's chest where the lungs should be. The baby's heart may also be pushed to one side by the extra organs in the chest.
A prenatal ultrasound that suggests CDH should be further evaluated by a high-volume fetal center.
Experience Matters
If you choose the Center for Fetal Diagnosis and Treatment at Children's Hospital of Philadelphia (CHOP), you will first speak with a knowledgeable fetal therapy nurse coordinator or genetic counselor who will answer your questions and schedule a comprehensive one-day evaluation. More than 1,609 patients with CDH have been referred to our team, experience that makes us uniquely equipped to evaluate and manage your baby's diagnosis.
Our team of dedicated imaging specialists uses the most advanced prenatal imaging techniques and state-of-the-art technologies available to gather detailed information about your baby's diagnosis.
- High-resolution fetal ultrasound to evaluate the CDH and overall fetal anatomy.
- Ultrafast fetal MRI, pioneered at Children's Hospital of Philadelphia, will provide additional anatomic details about the CDH as well as measure lung volumes.
- Fetal echocardiogram will evaluate heart structure and function.
These specialized tests help us determine which side of the diaphragm is affected by the CDH (left, right, or both), which organs are in the chest (stomach, intestines, and/or liver), and also measure the lungs to guide how the baby could be impacted after birth.
Determining severity of CDH before delivery
 This ultrafast fetal MRI confirms liver herniation into chest The strongest prediction of the severity of CDH is the location of the liver. When the liver is up in the chest there is more pulmonary hypoplasia (small lungs). The degree of pulmonary hypoplasia can be predicted by measurements obtained during the fetal ultrasound and MRI.
This ultrafast fetal MRI confirms liver herniation into chest The strongest prediction of the severity of CDH is the location of the liver. When the liver is up in the chest there is more pulmonary hypoplasia (small lungs). The degree of pulmonary hypoplasia can be predicted by measurements obtained during the fetal ultrasound and MRI.
- Lung area to head circumference ratio (LHR)
- Lung area to head circumference observed to expected (LHR O/E)
- Total lung volume observed to expected (MRI O/E)
While these calculations provide a volume (size) assessment of the developing lungs they can't predict the degree of pulmonary hypertension which affects how well the lungs will work after birth. (For clinicians: CDH diagnostic tool)
Left CDH or right CDH: What is the difference?
Approximately 83% of babies with CDH have a defect on the left side of the diaphragm. A left-sided CDH allows for the possibility of the stomach, intestines, and sometimes the liver to move (herniate) up into the baby's chest.
The other 17% of babies with CDH have a defect on the right side of the diaphragm. A right-sided CDH almost always allows the liver to move into the chest. Learn more about the treatment approaches and outcomes of left vs. right CDH.
To ensure an accurate diagnosis, it is important to visit a fetal therapy center with a multidisciplinary team experienced in evaluating pregnancies affected by CDH. This is an important step in determining the available treatment options and ensuring the best possible outcomes for your child.
To help you make decisions about your child's care, we encourage you to read these frequently asked questions about CDH, where we answer some of the most common questions families ask.
After all testing is complete, our team, led by a maternal-fetal medicine specialist and a pediatric surgeon both with experience managing pregnancies affected by CDH, meets with you and your family. Together we review imaging and test results, discuss the diagnosis, explain treatment options and potential outcomes, and answer any questions you may have.
You will typically be seen every four weeks for follow up until later in pregnancy when you'll be seen more frequently by an obstetrical team experienced in managing pregnancies affected by CDH and led by a maternal-fetal medicine specialist. During your follow up ultrasounds the lung measurements will be updated, your baby's growth will be carefully watched, and the amount of amniotic fluid around the baby will be measured. Weekly testing begins at 34 weeks to closely monitor fetal well-being.
At this time, relocation is necessary if you live more than one hour away from our center. You will need to relocate sooner if you undergo prenatal intervention, if extra fluid develops around your baby (polyhydramnios), or if there are signs of preterm labor. This will ensure that you are nearby in the event labor occurs or delivery is indicated earlier than expected. Our social workers will help coordinate housing options based upon your family's needs.
Watch the video to follow one family's journey from prenatal diagnosis of CDH through discharge home, and learn more about why it's important to seek care from an experienced CDH center.
View this video with a transcript
Fetoscopic endoluminal tracheal occlusion (FETO) is a fetal surgery procedure that may improve outcomes in babies with severe cases of CDH.
Hope for Severe Cases
In severe cases, CDH can lead to serious disease and death at birth. For these babies, treatment before birth may allow the lungs to grow enough before birth so these children are capable of surviving and thriving. Your maternal-fetal medicine physician and pediatric surgeon will discuss this treatment option with you during your evaluation to determine if it may be appropriate for your baby.
The health of a baby born with CDH can change unexpectedly, making it critically important to deliver within the hospital where postnatal care will be received and have all aspects of specialized care immediately available in one location.
You can expect delivery around 38-39 weeks for your baby with CDH. Most babies with CDH are born vaginally unless there are obstetric indications for a cesarean delivery. Your maternal-fetal medicine team will discuss delivery options with you. You will deliver your baby in CHOP's Garbose Family Special Delivery Unit (SDU), specially designed to keep mother and baby together in the same hospital and avoid transport of fragile infants.
At delivery, your baby is cared for in an adjoining room where the Newborn/Infant Stabilization Team and Neonatal Surgical Team — including neonatologists, surgical advanced practice nurses, neonatal and surgical fellows, neonatal surgical nurses, and respiratory therapists — are waiting to stabilize your baby.
Your baby will immediately have a breathing tube placed and will be connected to a ventilator (breathing machine). They will also have a tube placed into the nose (NG) or mouth (OG) to the stomach to keep it decompressed so the lungs have room to expand during breathing. The baby will be treated with "gentle ventilation" which is a specialized technique of providing breathing support to babies with CDH.
The baby will also have special lines placed into the blood vessels of the umbilical cord to monitor different blood levels and provide fluids and medications. Additional intravenous lines will be placed in the baby's hands or feet if needed. Once the baby is stabilized the team will bring the baby to you before transporting them to the Newborn/Infant Intensive Care Unit (N/IICU) for further care.
Parents are a vital part of the baby's team. You will have 24-hour access to your baby during their N/IICU stay, and we encourage your presence and interaction with your baby as much as possible.
For babies born with CDH, every little detail matters and can impact the outcome. It is important that your baby be treated by a team with experience caring for babies with CDH.
Finding Hope at CHOP
At CHOP, we see nearly 50 babies every year with CDH — more than anyone in the U.S. Our Neonatal Surgical Team is the only team of its kind in the world, working together since 2004. Your baby will be cared for using optimal care guidelines developed by our experienced multidisciplinary team.
In addition to surgical repair, your baby's CDH treatment may include specialized equipment such as the oscillator ventilator, heart lung machine (ECMO) or nitric oxide. Even if they don't need these options, it is important that they have immediate access when necessary.
N/IICU stay for babies with CDH
Your baby will be settled into the N/IICU where the initial goal is to keep the baby as stable as possible. Lights will be kept low; noise and handling will be minimized to optimize functioning of the baby's small lungs which are highly reactive to stimulation because of the associated pulmonary hypertension.
If the baby doesn't respond well to initial ventilation, the mode of ventilation can be changed to high-frequency oscillatory ventilation (HFOV) which delivers breaths and pressure differently than a conventional ventilator.
ECMO
If the baby is unstable, they may move onto extracorporeal membrane oxygenation (ECMO).
ECMO allows the lungs to rest while a machine takes over the function of the heart and the lungs, delivering oxygen to the baby while removing carbon dioxide, the waste product of breathing.
Excellence in ECMO
The ECMO Center at CHOP has been designated a Center of Excellence by the Extracorporeal Life Support Organization since 2008. We have had more than 1,500 ECMO cases since opening in 1990, and have supported nearly 250 babies with CDH.
Congenital diaphragmatic hernia repair
Surgical repair of CDH after delivery depends on your individual baby's progress in the days following birth.
The multidisciplinary team, led by your baby's pediatric surgeon and neonatologist, will determine the timing of repairing the defect in the diaphragm. In our experience it is best to wait until the lungs show less resistance from the pulmonary hypertension and the baby has transitioned off ECMO. Our experienced team utilizes various medications and inhaled therapy to enhance this process.
Babies with CDH are extremely sensitive to noise and movement, so surgical repair of CDH is often performed in the N/IICU. When it is time for the repair, the surgical team transforms your baby's N/IICU bedside into an operating room. This eliminates the additional stress to the baby of having to be transported.
Your baby will receive general anesthesia and will be monitored by a pediatric anesthesiologist. An incision is made just below your baby's rib cage, the organs in the chest are guided back down into the abdomen and the hole in the diaphragm is sewn closed. The space created in the chest allows the lungs to continue to grow.
For babies with large defects or completely lacking a diaphragm, the hole is closed with a GORE-TEX® patch or muscle flap. As your child grows, the condition of the patch will be regularly monitored by doctors to ensure that it remains intact.
Congenital Diaphragmatic Hernia (CDH) Surgical Repair
-
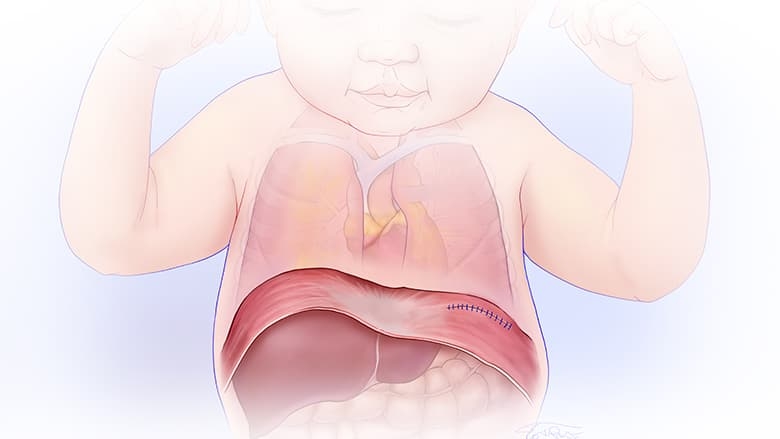
After gently bringing the liver, stomach and intestines into place, surgeons repair the hole in the diaphragm, using stitches to sew together the muscles.
-
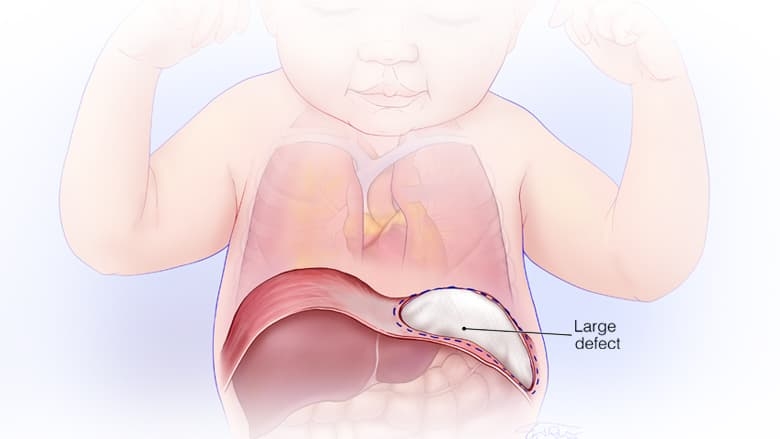
Often, a Gore-Tex patch is used to close larger openings.
1 of 1
Recovery after CDH surgery
Your baby will recover from surgery and begin the process of weaning from the ventilator. Once the baby is ready, feedings of either breast milk or formula will slowly begin through the NG or OG tube. When the breathing tube is removed a speech therapist and lactation consultant will work with your baby to start feeding by mouth.
The length of your baby's hospital stay from birth to discharge is largely dependent on the severity of your baby's CDH and their response to treatment. As babies receive this comprehensive medical care, social workers and psychologists help support family members through all the ups and downs you experience.
Once your baby is discharged home we will schedule them for follow up care in our Pulmonary Hypoplasia Program (PHP). Your baby will meet with multiple specialists in one location to monitor and treat any needs related to the CDH. Learn more about the long-term care provided by our PHP team.
Long-term follow-up by a team of experts is important to provide the best clinical care to your child. Children's Hospital of Philadelphia's unique Pulmonary Hypoplasia Program (PHP) provides comprehensive, interdisciplinary follow-up care for children with CDH. The team is made up of clinicians from general surgery, developmental pediatrics, pulmonary, cardiology, psychology, nutrition, audiology, social services and others as needed.
The PHP follows nearly 600 children with CDH well into school age. Initial follow-up by the PHP will be arranged when your baby is in the N/IICU. Appointments are tailored to your child's needs, but typically occur at 6 months, 12 months, 2 years, 4.5 years and 6 years, and then every 2 years thereafter, as needed. Appointments are designed for visits to multiple specialists in one day.
CHOP is committed to comprehensive evaluation over your child's lifetime so that we can continuously improve care and understand long-term outcomes.
Most babies with CDH cared for by CHOP meet expected growth and developmental milestones by kindergarten. Some children will need ongoing support through the PHP to optimize outcomes. Our team is here for you every step of the way.
Should Diaphragmatic Hernia Be Repaired If No Symptoms
Source: https://www.chop.edu/conditions-diseases/congenital-diaphragmatic-hernia-cdh
Posted by: bakerfacesoccat.blogspot.com

0 Response to "Should Diaphragmatic Hernia Be Repaired If No Symptoms"
Post a Comment